Eye Eyelid Lacrimal Gland Eye
The eye is the organ of vision. It is spherical and has the following three coats:
- Fibrous coat – Sclera and cornea
- Vascular coat – Choroid, ciliary body and iris
- Nervous coat – Retina
The transparent structures in the path of light are the cornea, aqueous humour (of the anterior chamber), the lens and the vitreous body (a gel-like substance in the posterior chamber).
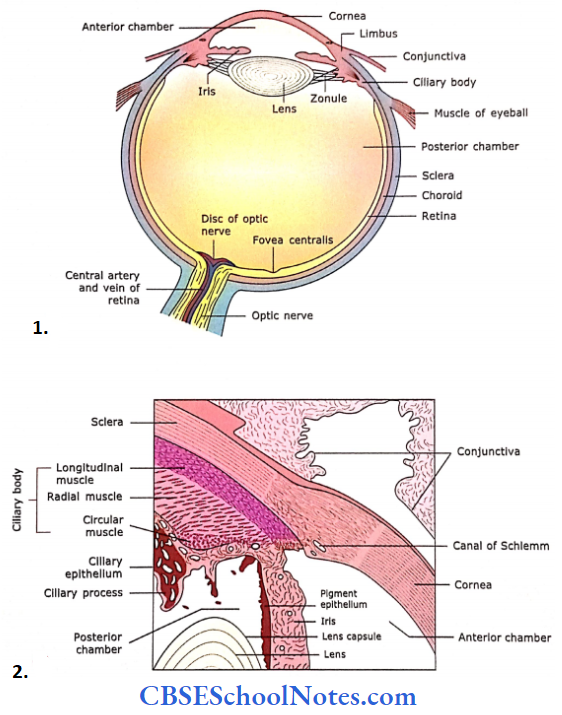
- The sagittal section of the eye shows Its gross structure.
- Schematic diagram showing sclerocorneal Junction, ciliary body and process, Iris and lens.
Fibrous Coat
Sclera
The sclera is a tough, fibrous connective tissue layer. It consists of irregularly arranged dense connective tissue, i.e., flat bundles of type 1 collagen fibres, a network of elastic fibres and fibroblasts. Its thickness ranges from 0.6 mm to 1 mm.
Cornea
The cornea is located at the front of the eye and is continuous with the sclera at the limbus. It is a transparent portion of the eye, hence, avascular.
It is about 1 mm thick and consists of five layers. From superficial to deep these are:
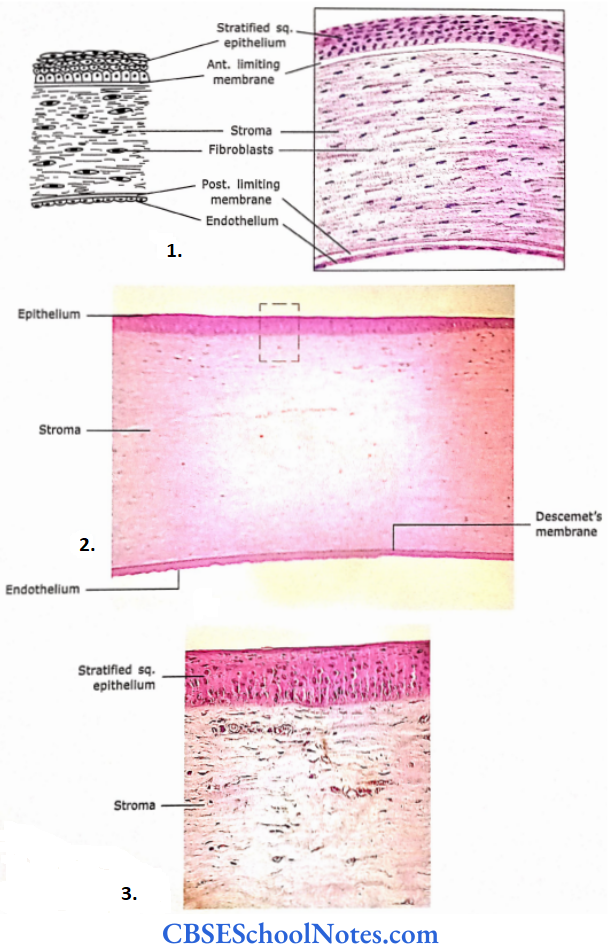
- Section of the human cornea showing various layers.
- Section of the cornea at low magnification.
- Photomicrograph at high magnification.
Corneal epithelium: It consists of stratified squamous, non-keratinized epithelium. Sensory nerves supply it. The cornea is very sensitive and any irritation or injury causes severe pain, excessive lacrimation, photophobia and blinking of eyelids.
Bowman’s membrane: It is about 10-12 mm thick, structureless, homogeneous lamina consisting of randomly oriented thin fibrils of collagen.
- This layer is also known as an anterior limiting membrane. It acts as a barrier to the spread of infection. It is believed that Bowman’s membrane is synthesized by both the corneal epithelium and underlying stroma.
- If damaged, it cannot regenerate. It heals by the formation opaque scar, which interferes with vision.
Corneal stroma: It constitutes the bulk of the cornea (90% of thickness). It is made up of thin lamellae of mostly type I collagen fibres, which are arranged in many layers.
- The bundles of collagen fibres, within a lamella, are highly ordered. In the adjacent lamellae, the bundle of collagen fibrils are arranged at a right angle to each other.
- The cornea is transparent because of the orderly arrangement of collagen fibrils. The flattened fibroblasts are located between the lamellae.
- The canal of Schlemm is present at the sclerocomeal junction (limbus). It is the site of the outflow of the aqueous humour from the anterior chamber of the eye into the venous system.
Descentet’s membrane: This layer is also known as a posterior limiting membrane. It is an acellular, homogeneous basement membrane consisting of interwoven meshwork of collagen fibrils. It is a product of endothelium.
Endothelium: It is a single layer of squamous or low cuboidal cells on the posterior surface of the cornea, resting on Descemet’s membrane.
- All the metabolic exchange between the cornea and aqueous humour takes place through the endothelium. It is responsible for the synthesis of proteins, which are necessary for maintaining Descemet’s membrane.
- It also reabsorbs excessive fluid from the stroma to keep it relatively dehydrated, which helps in the refractive quality of the cornea.
Fibrous Coat Remember
The cornea is a transparent avascular membrane. It consists of two noncellular layers (Bowman’s membrane and Descemet’s membrane) and three cellular layers (corneal epithelium, corneal stroma and endothelium).
If Bowman’s membrane is damaged, it cannot regenerate. It heals by the formation of an opaque scar, which interferes with vision. Descemet’s membrane is an unusually thick basement membrane for a very thin endothelial lining.
Fibrous Coat Clinical Applications
Corneal Transplants
- If a person has a defective cornea (presence of opacity), it interferes with normal vision. This cornea may be removed and a normal cornea obtained from a dead person (through eye donation) can be transplanted.
- Corneal transplants are the most common and successful organ transplants. This is because the cornea is an avascular tissue.
- Hence, antibodies that may cause rejection of transplanted cornea do not enter the transplanted tissue.
Glaucoma
The failure of drainage of aqueous humour from the anterior chamber of the eye leads to a prolonged increase in the intraocular pressure. The condition is known as glaucoma. It is an important cause of blindness.
Vascular Coat
The vascular coat consists of a choroid, ciliary body and iris.
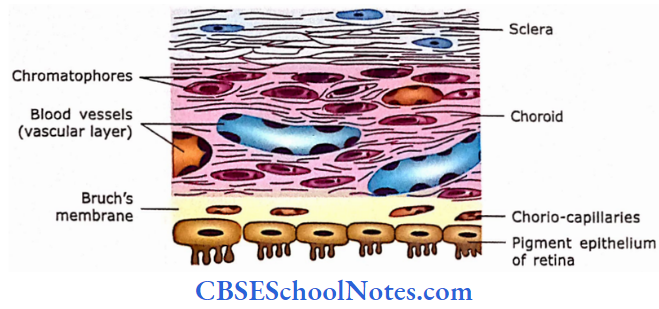
Choroid
The choroid is the posterior portion of the middle coat of the eyeball. It is the thin, highly vascular layer that lies between the sclera and retina. It consists of four layers:
- Suprachoroid layer: This layer consists of fine collagenous fibres, elastic fibres and pigment cells (chromatophores).
- Vascular layer: This layer consists of large blood vessels between loose connective tissue and pigment cells.
- Chorio-capillary layer: This layer consists of a capillary network, which is essential for the nutrition of the retina.
- Bruch’s membrane: This membrane separates the choroid from the retina. It is a thin (1-4 mm) refractile membrane. It also acts as the basal lamina for the pigment cell layer of the retina.
Vascular Coat Remember
The choroid is a pigmented vascular layer, which lies between the sclera and the retina. It is separated from the retina by Bruch’s membrane.
Ciliary Body
The ciliary body is made up of ciliary muscle (smooth muscle) and ciliary process. The smooth muscle of the ciliary body is oriented in longitudinal, radial and circular directions.
- The ciliary muscle alters the shape of the lens for near and far vision. From the ciliary body, there come out 60-70 short ciliary processes with suspensory ligaments of the lens.
- The ciliary processes are covered by bi-laminar epithelium and have a core of loose connective tissue and blood vessels.
- The outer cell layer is the non-pigmented columnar epithelium, whereas the inner cell layer is composed of a pigmented simple columnar epithelium. The ciliary epithelium produces aqueous humour.
Ciliary Body Remember
The ciliary body is the anterior part of the vascular coat. It is located between the iris and the choroid. The ciliary body is made up of ciliary muscle (smooth muscle) and ciliary process.
The smooth muscle of the ciliary body is oriented in longitudinal, radial and circular directions.
Iris
The iris arises from the ciliary body and lies between the cornea and the lens. It consists of smooth muscle fibres in the connective tissue stroma (fine collagen fibres), melanocytes and blood vessels.
- It has no epithelium on its anterior surface, but the posterior surface of the iris is lined by ciliary epithelium. This layer is heavily pigmented and the colour of the eye depends on its pigmentation.
- The smooth muscle of the iris is arranged in two layers, i.e., dilator pupillae and sphincter pupillae. The dilator pupillae fibres are radially oriented.
- While sphincter pupillae are oriented circumferentially near the pupil. Iris acts as a diaphragm, which controls the amount of light entering the eye.
Iris Remember
The iris is the anterior extension of the vascular coat. It acts as a diaphragm, which controls the amount of light entering the eye.
Nervous Coat
Retina
This is the inner coat of the eyeball and lines its posterior surface. The retina contains photoreceptors (rods and cones), which are essential for vision. The retina has a specialized area where vision is most acute, the fovea centralis or macula.
- This area contains only cones, which are essentially bare (the overlying layers are pushed to the side). The retina also has a ‘blind spot,’ the optic disc.
- Where the optic nerve leaves the eye and there are no photoreceptor cells. The retina has several layers from the outside in the following.
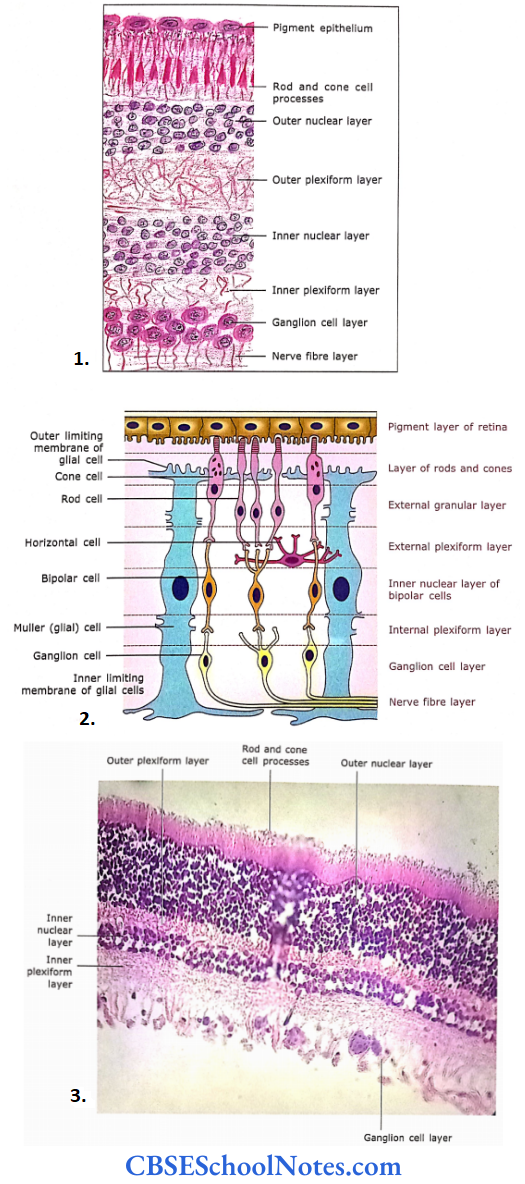
- The microscopic structure of the retina.
- Diagrammatic representation of principal cell types of the retina and their connections.
- Photomicrograph of the retina at high magnification.
Pigment Epithelium
It is the outermost layer of the retina, which is separated from the choroid by Bruch’s membrane. This epithelium consists of low cuboidal cells, which contain melanin granules.
- Epithelial cells have long apical processes that occupy spaces between the outer segment of rods and cones.
- The melanin pigment of epithelium absorbs light, thus preventing its reflection from the outer coats of the eye. The pigment epithelium also phagocytizes the tip of rod and cone cell processes.
Layer of Rod and Cone Cell Processes
This layer consists of outer segments of rod and cone cells. The processes of rod cells are cylindrical and cones are thicker, cone-shaped. This layer is a photoreceptor in function.
- Rods and cones are photoreceptor cells. They transfer the light energy into receptor potential. Both types of cells are long slender cells but the outer segments of rods are cylindrical or rodshaped
- Whereas those of cones are tapered or cone-shaped. The rod cells are much more in number [120 million] compared to cone cells [6 to 7 million]. The parts of rod and cone cells are shown.
- The rod consists of the outer segment, inner segment, inner fibre and spherule. The parts of the cone cell are almost the same except the terminal part is called the pedicle, instead of the spherule.
Outer Nuclear Layer
This layer consists of nuclei belonging to rods and cones. The nuclei of these cells are arranged in several layers. This layer is darkly stained.
- Between the second and third layers, there is the presence of a pink linear marking called an outer limiting membrane or lamina.
- This results because of zonula adherens of the glial cells (Muller cells) with the cell bodies of photoreceptor cells.
- The Muller cells are supporting cells of the retina. They have long slender bodies that are radially oriented in the retina.
Outer Plexiform Layer
This layer stains lightly. The layer contains synapses between rods and cones with the dendritic processes of bipolar cells and horizontal cells.
Inner Nuclear Layer
It consists of cell bodies and nuclei of bipolar cells, horizontal cells, amacrine cells and Muller’s cells. The bipolar cells are oriented perpendicular to the layers of the retina.
- They have synaptic contact with rod or cone cells at the outer (dendritic) end and with ganglion cells at the inner (axonal) end. The horizontal cells are oriented parallel to the layers of the retina.
- Their processes form synaptic contact with rod and cone cells in the outer plexiform layer.
- The amacrine cells are situated in the inner portion of this layer and have synaptic contact with axonal processes of bipolar cells and dendrites of ganglion cells in the inner plexiform layer.
Inner Plexiform Layer
In this layer, the axons of bipolar cells synapse with dendrites of ganglion cells and amacrine cells.
Ganglion Cell Layer
Mainly consists of the body and nuclei of large multipolar neurons (ganglion cells). They receive input from bipolar cells and their axons form optic nerve.
Nerve Fibre Layer
It consists of central processes (axons) of ganglion cells, which gather at the optic papilla (disc) and leave the eye as the optic nerve. As soon as these fibres leave the eyeball, they become myelinated.
The blood vessels of the retina are present only in the nerve fibre layer. However, sometimes they may reach as deep as the outer nuclear layer.
Nerve Fibre Layer Remember
The retina consists of ten layers of cells and their processes. Road and cone cells of the retina are specialized photoreceptors. Roads are specialized to perceive dim light, while cone cells perceive bright light and colour.
Nerve Fibre Layer Clinical Application
Detachment of Retina
As the apical ends of rods and cone cells are not firmly attached to the pigment epithelium, the retina may get separated from the pigment epithelium. This condition is called detachment of the retina.
- This is a common but serious condition. It may be treated by laser surgery. If it remains untreated, rods and cones are damaged, leading to blindness.
- This is because rod and cone cells get their nutrition from a chorio-capillary layer of choroid.
Lens
The lens is a transparent, flexible, biconvex disc. The lens is involved in near and distant vision, which is achieved by changing its curvature. The lens consists of a lens capsule, anterior epithelium and lens substance.
Lens Capsule
The lens is covered by a lens capsule, which is a homogeneous basal lamina coat. The capsule is made up of type 4 collagen and proteoglycans.
Anterior Epithelium
Beneath the capsule, simple cuboidal epithelium covers the anterior surface of the lens.
Lens Substance
The anterior epithelial cells toward the equator become columnar. The columnar cells of the equatorial region further elongate to form long fibres.
- These long fibres are about 7-10 mm in length, 8-12 pm wide and 2 pm thick. In the cross-section, their shape is like a hexagon.
- Although these fibres are called lens fibres, they are in a true sense modified elongated epithelial cells. The younger fibres are nucleated, whereas old fibres lose their nuclei.
Lens Substance Clinical Application
- Cataract
- The entire lens substance consists of transparent lens fibres. However, with increasing age or metabolic disorders (diabetes), the lens may become opaque.
- This interferes with clear vision. This condition is called a cataract. In this condition, the lens is removed from its capsule and replaced with a plastic lens.
- Presbyopia
- The lens is highly elastic. However, the elasticity of the lens is gradually lost due to increasing age. This leads to difficulty in accommodation for near objects (reading, etc).
- This is usually observed after 40-45 years of age. The condition (presbyopia) is corrected by wearing glasses with a convex lens.
Eyelid
The eyelids protect the eye. From external to internal surface eyelid consists of many layers, i.e., skin, loose connective tissue, orbicularis oculi muscle, tarsal plate and palpebral conjunctiva.
- The skin of the eyelid is thin, loose and elastic.
- The loose connective tissue is present deep in the skin, which is devoid of fat.
- The third layer of the eyelid is formed by bundles of skeletal muscle (orbicularis oculi). The tarsal plate is made up of dense connective tissue and forms the skeleton of the eyelid.
- The inner surface of the lid is lined by palpebral conjunctiva. The palpebral conjunctiva consists of stratified columnar epithelium with goblet cells.
There are three types of glands present in eyelids.
- Tarsal glands (Meibomian glands) are long sebaceous glands, which are present in the tarsal plate.
- They produce sebaceous secretion, which forms an oily layer on the surface of the ear, thus preventing an early evaporation of tears.
- Glands of Zeis (sebaceous gland of the eyelid) are small modified sebaceous glands, which are connected with the follicles of eyelashes.
- Glands of Moll are small sweat glands that pour their secretion into eyelashes. They are simple spiral tubular glands.
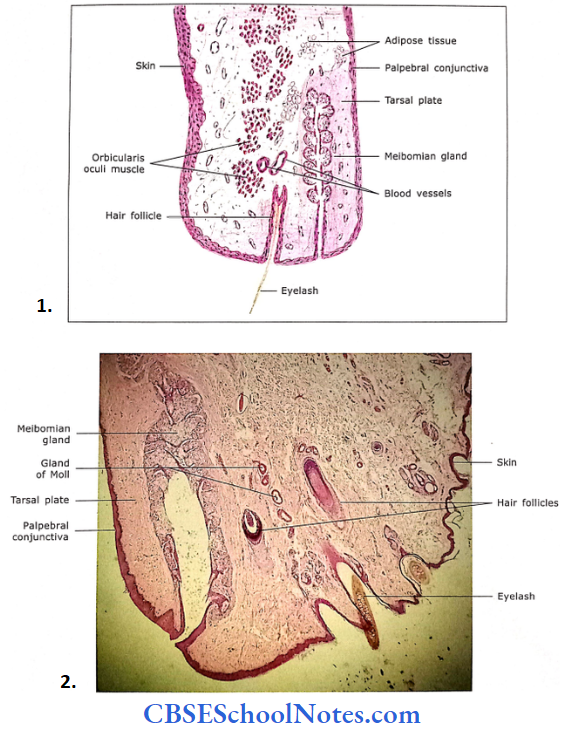
- Histological structure of eyelid.
- Section of eyelid.
Eyelid Remember
The main function of eyelid is to protect the eye. On its outer surface, it is covered by skin and its inner surface is covered by palpebral conjunctiva. Three types of glands are present in the eyelid.
Lacrimal Gland
The lacrimal gland is a compound tubuloacinar serous gland. It consists of many separate lobes, which pour their secretion (tears) in the superior conjunctival fornix through small ducts.
- The lacrimal gland acini has the features of a serous salivary gland. These acini are lined by light-staining low columnar cells.
- The acini are large and have a wider lumen compared to the serous salivary gland.
Myoepithelial cells are located within the lamina of acini and help in the release of tears.
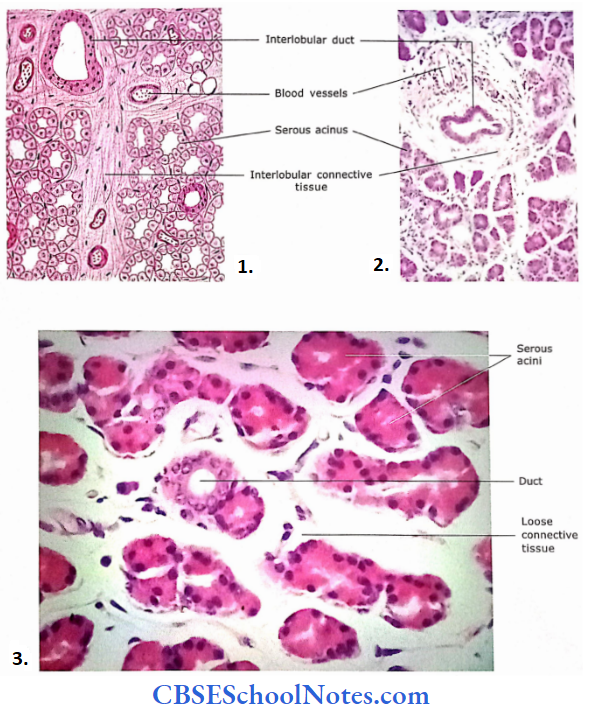
- Section of lacrimal gland.
- Lacrimal gland as seen under low magnification.
- Magnified view of lacrimal gland
